The Role of RT-PCR in COVID-19 Testing
Polymerase chain reaction (PCR), the enzymatic method of replicating DNA sequences, is used to detect and amplify a specific DNA sequence. Reverse Transcription PCR (RT-PCR) combines the reverse transcription of RNA into complementary DNA (cDNA) with DNA amplification using PCR. RT-PCR uses RNA as a template and starting material for nucleic acid amplification. RT-PCR is commonly used to diagnose and quantify RNA virus infections, such as the recent SARS-CoV-2 virus.
RT-PCR can also be combined with quantitative PCR (qPCR) to measure the quantity of cDNA as it accumulates in the reaction after each amplification cycle. The transcription ability in RT-qPCR is used in various applications such as gene expression analysis, RNAi validation, pathogen detection, and disease research. Both techniques are utilized in COVID-19 diagnostic testing and research.
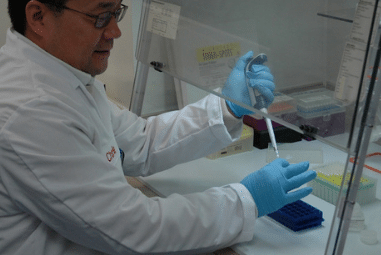
In COVID-19 diagnostic testing, RT-PCR is used to detect the presence of the virus in the patient’s body. The genome of SARS-CoV-2 is encoded in a single-stranded RNA. Therefore, all RNA in the patient’s swab sample must be extracted using an appropriate nucleic acid preparation method. Then, all of the isolated RNAs are converted to cDNAs using the reverse transcriptase enzyme. From here on, PCR is used to amplify and detect a specific DNA molecule, which is the viral cDNA of interest. In PCR, these double-stranded DNAs are first separated in the denaturation process. Next, a specific primer that will only attach to the viral cDNA is added into the mix. The specificity of the primers ensures that they only bind to the viral cDNA and not to any other cDNA present in the sample. In the final step, a polymerase enzyme is used to add nucleotides to the ends of the primers, which elongates the separated cDNA strands into two complete double-stranded cDNAs. This process is repeated in cycles to amplify the DNA to the required DNA amount for detection and further analysis. This detection stage determines whether or not the SARS-CoV-2 virus is present in the patient’s swab sample.
The qPCR aspect can be added into this process by introducing a specific probe which will give fluorescence whenever a new DNA molecule is formed. With this probe, the increase of viral cDNA produced can be tracked in real-time by monitoring the increase in fluorescence signal. When the signal exceeds a certain threshold, we can be confident that the viral cDNA presence is significantly higher than the background noise. The cycle threshold (Ct) is the number of cycles required for the signal to exceed the threshold. A low Ct number indicates a high amount of RNAs present in the sample, as it only needs a few cycles for the signal to exceed the threshold. Therefore, a low Ct number also represents a higher viral load in the original sample. For SARS-CoV-2, a Ct number below 40 is considered a positive test. Many studies suggest that the lower the Ct number, the higher the chance for the patient to develop a more severe COVID-19 disease, as they must have more viral particles in their body.
The high specificity of the RT-PCR kits is essential to minimize the false positive and, more importantly, false negative in COVID-19 diagnostic tests. This technique can produce test results in a matter of hours, which is critical for rapid and high throughput testing. Therefore, demand for this technology sky-rocketed in 2020 due to the dire need for COVID-19 rapid testing and tracking in order to reduce the spread. Aside from the instrumentation, sales of RT-PCR and RT-qPCR reagents and kits involved in COVID-19 diagnosis are expected to spike in the short term. However, this vigorous growth will rapidly recede once effective vaccination against SARS-CoV-2 becomes widely available. The details of this exciting market dynamic can be found in SDi’s latest publication, the Global Laboratory Consumables Market 2020 report. The report analyzes both analytical and life science consumables for global market sizing along with segmented forecasts, vendor share, and other information.